Hashimoto’s Mechanisms of Action, and how Traditional Chinese Medicine Can Help
Understanding the Underlying Mechanisms of Hashimoto’s Thyroiditis
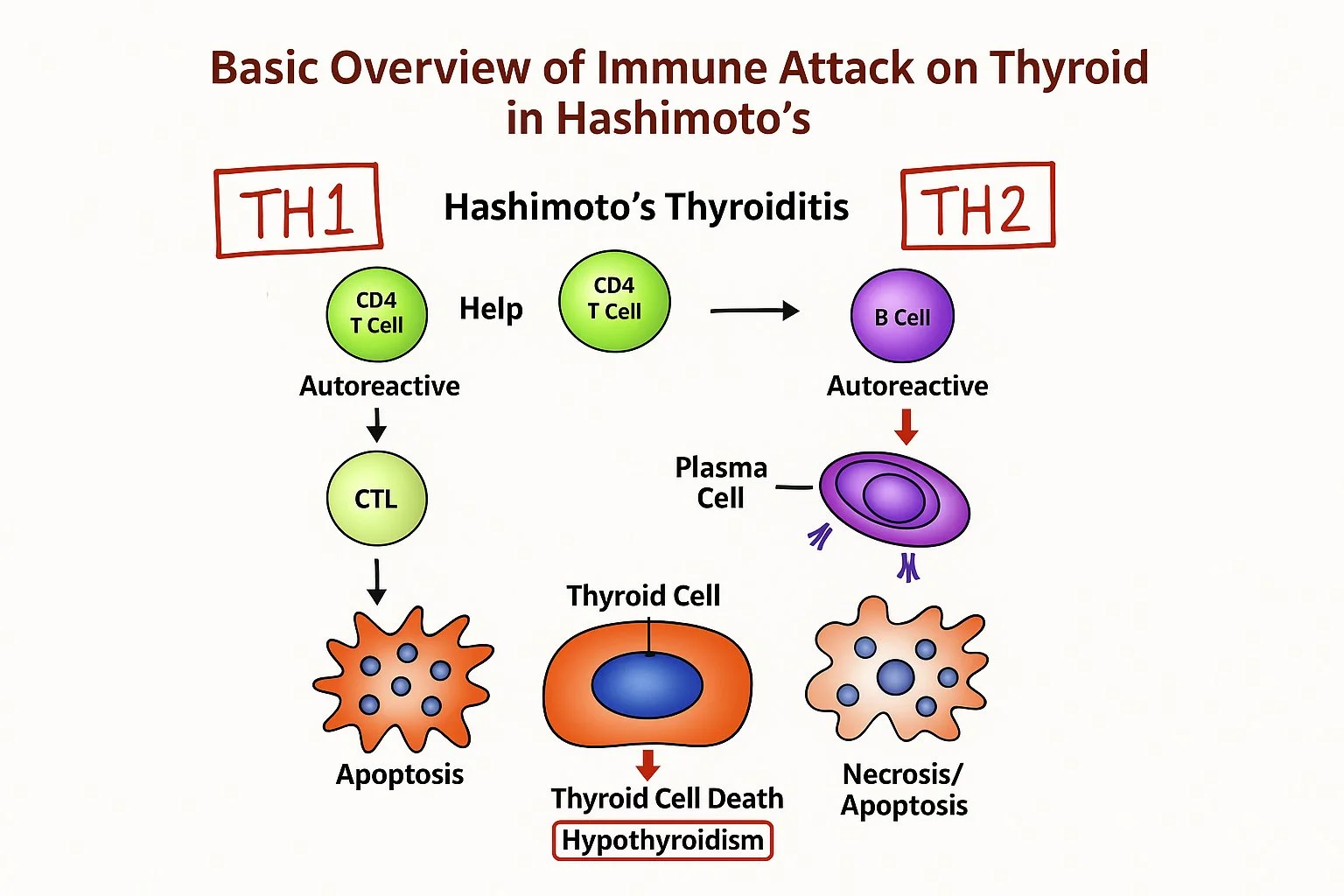
Hashimoto’s thyroiditis is the most common autoimmune thyroid disorder in the U.S., and its mechanisms are complex. At its core, Hashimoto’s involves an immune system malfunction in which both the cellular (TH1) and humoral (TH2) branches of immunity begin to target the thyroid gland. Specifically, TH1-dominant immune responses lead to the destruction of thyroid follicular cells through antibody-mediated and cytotoxic T-cell pathways. These immune cells either attack the thyroid directly or release cytokines that disrupt the metabolic and immune function of thyroid cells. Over time, this process leads to a gradual decline in thyroid hormone production, eventually resulting in hypothyroidism and associated symptoms like fatigue, weight gain, cold sensitivity, and reproductive challenges.
Contributing to this autoimmune cascade are three essential components:
a genetic predisposition
environmental triggers
intestinal permeability (or “leaky gut”)
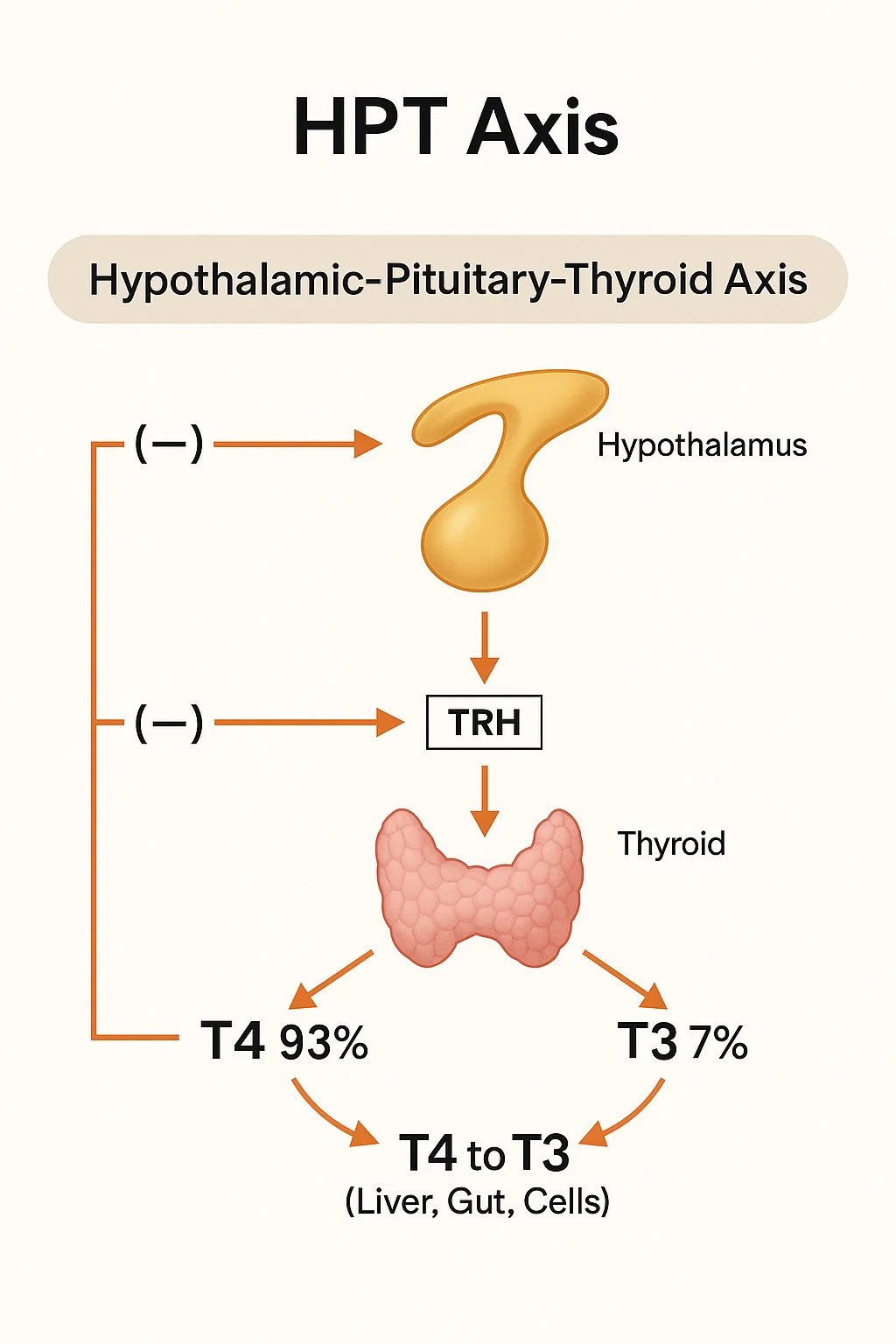
This triad creates the perfect storm that disrupts immune tolerance and initiates a chronic, self-perpetuating inflammatory response. From a physiological standpoint, Hashimoto’s compromises the Hypothalamic-Pituitary-Thyroid (HPT) axis, disrupting the delicate hormonal signaling needed for balanced thyroid function. Additionally, essential biochemical processes - like iodine uptake, tyrosine synthesis, thyroid peroxidase enzyme activity, and conversion of T4 to T3 - can become impaired, further reducing the thyroid’s ability to meet the body’s metabolic needs.
This autoimmune process doesn’t occur in isolation. Hashimoto’s frequently coexists with other conditions, such as infertility, depression, and gut dysbiosis, and can impact multiple systems in the body. Understanding these underlying mechanisms allows for a more holistic and effective treatment strategy, one that addresses not just the thyroid, but the broader immune, digestive, and endocrine imbalances contributing to the condition.
The Primary Thyroid Markers
TSH (Thyroid Stimulating Hormone): elevated TSH indicates your pituitary gland is working harder to stimulate an underactive thyroid
Free T4 (Free Thyroxine): measures the active, unbound thyroid hormone available for your body to use. Low Free T4 levels confirm hypothyroidism when combined with high TSH
Free T3 (Free Triiodothyronine): the most active form of thyroid hormone. Abnormal values can indicate a problem with T4 to T3 conversion
Anti-Thyroid Peroxidase antibodies (TPO): elevated in over 90% of Hashimoto's patients; indicates an autoimmune component
Thyroglobulin antibodies (TgAb): may also be elevated in Hashimoto's and also helps confirm an autoimmune component
Hashimoto’s and Reproductive Health
The thyroid antibodies (TPO and TgAB) that are elevated in Hashimoto’s patients are the primary culprits when it comes to how Hashimoto’s directly affects fertility. These antibodies don't just stay in the thyroid, they cross into follicular fluid where eggs develop and their presence directly correlates to reduced fertilization rates, poorer embryo quality, and lower pregnancy rates. Furthermore, TPO antibodies are expressed in ovarian tissue, the endometrium, and the placenta, and when they attack these reproductive tissues they cause extensive damage and destroy healthy reproductive cells the same way they attack and destroy healthy thyroid cells.
This attack on the body creates a state of systemic immune system dysregulation and a self-perpetuating inflammatory cascade. Biologically, pro-inflammatory cytokines like TH17, TNF-α, and interferon-γ are upregulated while protective regulatory T cells (Treg) are reduced. This high inflammatory environment directly impairs oocyte quality, follicle development, and endometrial receptivity. Additionally, natural killer (NK) cells become hyperactivated, which normally help with implantation but in excess can attack embryos and reduce the chances of successful pregnancy.
TCM Intervention
There are several pathways by which acupuncture helps recalibrate these inflammatory markers and restore proper immune response. A 2022 study found that acupuncture significantly reduced TH1-specific cytokines including TNF-α and other inflammatory markers, while modulating Th17-specific cytokines like IL-17. Most importantly, the study showed acupuncture could rebalance TH1/TH2 and TH17/Treg ratios, which are fundamentally disrupted in Hashimoto's. A 2021 comprehensive review demonstrated that acupuncture enhances Treg function while suppressing pathogenic TH17 responses. The study showed acupuncture upregulates Treg markers like the anti-inflammatory cytokine IL-10, while downregulating TH17 cytokines including IL-17α. This is particularly relevant to Hashimoto's patients, where the loss of Treg suppressive function allows autoimmune attack on thyroid and other tissues.
Chinese herbal medicine can also have profound effects on Hashimoto’s management at the molecular level. Traditional herbal formulas such as Yang He Tang and Jie Yu Xiao Yin have been demonstrated to significantly restore the TH17/Treg balance by increasing the percentage of regulatory T cells while decreasing TH17 cell proportions, decreasing pro-inflammatory cytokines IL-6, IL-17, and TGF-β, and dramatically reducing TPO and TgAB antibodies. These studies provide robust evidence that TCM herbal formulas can specifically target the immune dysregulation and inflammatory cascade and reduce the antibody-mediated damage that compromises ovarian reserve and fertility in Hashimoto's patients, offering scientifically-validated options that can be used alongside conventional treatment approaches.