Metabolic Health, Infertility, and the Power of Acupuncture
Many years ago, I sat in a fertility acupuncturist’s office, anxiously searching for answers to my unexplained infertility. After reviewing my health history, the acupuncturist looked at me and firmly said, "Nothing is going to improve until we work on your egg quality. And the key to that is tackling your insulin resistance." The words landed with a thud. In that moment I knew, deep down, that she was right. With a family history of diabetes and lingering suspicion that I was genetically predisposed (or already prediabetic), it was a truth I hadn’t wanted to fully acknowledge, but her blunt conviction struck a chord I couldn’t ignore.
Have you ever had a moment where someone tells you something about your health and you just know it’s true in your bones? That’s how it felt. Instead of shying away from this realization I dove headfirst into the rabbit hole of research, discovering the myriad of ways in which insulin resistance and metabolic health affect not only egg quality, but all the ways it influences the entire delicate reproductive ecosystem.
Now, years later and after countless conversations with patients and peers, I see just how underrated insulin resistance is for those on a fertility journey. So let’s unpack why metabolic health is so central to reproductive success, and how therapies like acupuncture can be a powerful ally in course correcting metabolic regulation in the body.
What is Insulin Resistance?
At its core, insulin resistance occurs when our bodies start ignoring insulin, the hormone tasked with ushering glucose (sugar) into our cells to be used for energy. As the body becomes increasingly insensitive, it responds by producing more and more insulin to compensate. This high circulating insulin eventually begins to disrupt sex hormone balance, impairs how the ovaries function, affects the environment needed for healthy egg development, and reduces the uterine lining’s ability to support implantation.
Why Insulin Resistance Matters for Everyone
One of the clearest examples of this disruption is polycystic ovary syndrome (PCOS). Women with PCOS and metabolic dysfunction often find themselves tangled in a web of metabolic and reproductive challenges that include irregular or absent cycles, anovulation, heightened androgens, increased miscarriage risk, and weakened response to standard fertility treatments. But here’s something that isn’t always talked about - insulin resistance doesn’t just impact those with PCOS (I’m a perfect example of that). Women without a PCOS diagnosis, even those who aren’t overweight, can have subtle blood sugar dysregulation that silently undermines their fertility. Studies show that even in lean women undergoing IVF, higher degrees of insulin resistance are linked to fewer mature eggs, reduced embryo options, and an increased risk of pregnancy loss.
Genetics, Daily Habits, or Both?
Unfortunately, genetics play a huge role in determining how your body will respond to insulin over time. Variations in certain genes, specifically TCF7L2 and CRY1, can greatly influence our susceptibility to metabolic dysfunction. When these genetic predispositions combine with confounding factors like the modern American diet, a sedentary lifestyle, aging, chronic inflammation, environmental toxins, and prolonged periods of poor sleep or stress, the risk of developing insulin resistance rises substantially. Therefore, insulin resistance results from a complex interplay between our genes, environment, and daily habits.
Your Metabolism Directly Impacts Your Fertility
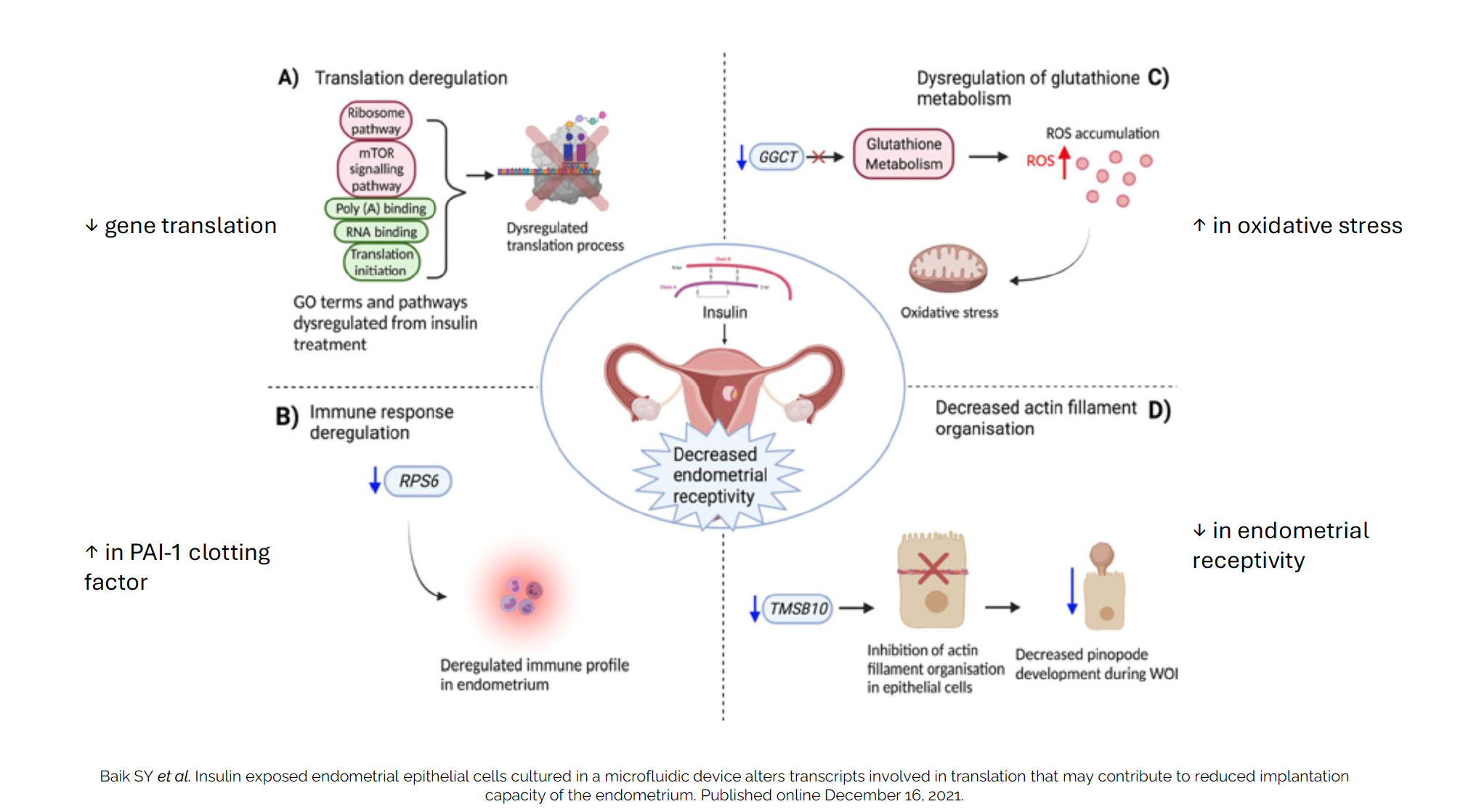
Mechanistically, insulin resistance strikes at multiple reproductive targets: the hypothalamus (altering crucial hormone signals), the ovaries (disrupting follicle development and oocyte maturation), the endometrium (making it less receptive to implantation), and even the eggs themselves (ratcheting up oxidative stress, fueling inflammation, and compromising their mitochondrial function). For patients, this means cycles that come and go without ovulation, lower chances with assisted reproductive technologies like IUI and IVF, and, sadly, heartbreak with recurrent miscarriage.
This is why knowing, and not shying away from, your own metabolic terrain is vital. While markers like HbA1c are commonly tested, they often capture problems only after they’re well established in the body. Earlier indicators (like fasting insulin, HOMA-IR, and oral glucose tolerance tests) can reveal hidden dysfunctions long before fasting glucose or standard labs turn abnormal. The earlier these are identified, the sooner intervention can begin.
Diet, Lifestyle, and Smart Supplementation
And what can be done? The backbone of any intervention plan is lifestyle, specifically tailored to the individual. The Mediterranean diet, rich in fiber, healthy fats, and plenty of plant-based nutrients, has repeatedly shown benefits for metabolic and reproductive health. Exercise doesn’t just burn calories; it increases insulin sensitivity, lowers inflammation, and improves hormonal signals. Strategic supplements, including inositols, N-acetyl cysteine (NAC), alpha-lipoic acid, berberine, and omega-3 fatty acids, are backed by growing evidence for improving both insulin sensitivity and reproductive outcomes, particularly in women with PCOS or metabolic dysfunction. If you’re interested in learning more about recommended fertility supplements, as well as how a customized treatment approach can benefit you, we can provide guidance as part of your individualized care plan.
A Bridge Between Metabolic Health and Fertility
So now let’s talk about acupuncture. Modern research supports its regulatory effects on the neuroendocrine system, which means that it directly influences the hormonal crosstalk between your brain, ovaries, and uterus. Through consistent, targeted treatments, acupuncture can help normalize menstrual cycles, support ovulation, and improve blood flow to the ovaries and uterus. But importantly, its benefits also extend to the broader context of metabolic health.
Acupuncture supports fertility and metabolic health by enhancing insulin sensitivity, reducing systemic inflammation and oxidative stress, and supporting better regulation of blood sugar, all of which improve fertility potential. Stress management is another hidden powerhouse: so many of my patients report substantially better mood, anxiety reduction, and better sleep after beginning acupuncture care, each of which plays into better hormonal and metabolic regulation.
The bottom line is that reproductive health and metabolic health are deeply intertwined. Insulin resistance is both reversible and manageable, but the earlier and more holistically you approach it, the better. My invitation to you: don’t be scared. Instead, see your fertility journey as an opportunity to get curious about your whole-body health and to use every supportive, evidence-based tool at your disposal. Acupuncture is a powerful option, but it works best as part of an integrated approach that centers on your unique story and biology.
If you have more individual questions, or just want to dig into your own health picture more deeply, Seed Acupuncture is always here to help. You don’t have to unravel this puzzle alone.